Basic Principles
BASIC PRINCIPLES OF CONVALESCENT PLASMA TREATMENT
PRINCIPLE #1: Patients should be treated early in the course of illness before it becomes too severe because that is when the patient benefits most from receiving antibodies.
- Out-patient treatment has been shown effective in a randomized trial in Argentina (Libster, et al, 2021).
- We recommend treating high-risk patients (the elderly, those with other health conditions) before admission to the hospital where this can be carried out. In the US, however, outpatient treatment is not yet authorized by the FDA.
For hospitalized patients, treat as early as possible – as soon as the decision to admit is made – initiate treatment in the emergency room. The focus for treatment should be on patients who are WHO4 (hospitalized, but not on oxygen or WHO5 (hospitalized on low flow oxygen) on the 11-point revised WHO scale.
PRINCIPLE #2: Use plasma with high antibody titers. Ideally, antibody titers should be > 1:160. The high antibody titer in infused plasma has been associated with lower mortality in non-ventilated patients (Joyner et al, 2021).
PRINCIPLE #3. Use an appropriate dose. For non-immunosuppressed patients, initially use 200 ml and consider repeating a 200 ml infusion in 24 hours if the patient is still symptomatic as per FDA guidance.
PRINCIPLE #4: Use locally procured plasma whenever possible because it is likely that the match of antibody to the viral strain that is locally active will be better (Kunze et al, 2021).
PRINCIPLE #5: Convalescent plasma is especially valuable in people who are immunosuppressed and who do not make antibodies to COVID-19 either when infected or when immunized. In such patients, treatment should be undertaken at any stage of illness and may have to be repeated frequently (Senefeld, et al 2021).
PRINCIPLE #6: Avoid the use of corticosteroids in patients not on oxygen, who are on low flow oxygen, or have C-reactive protein levels <12 (Keller et al, 2020).
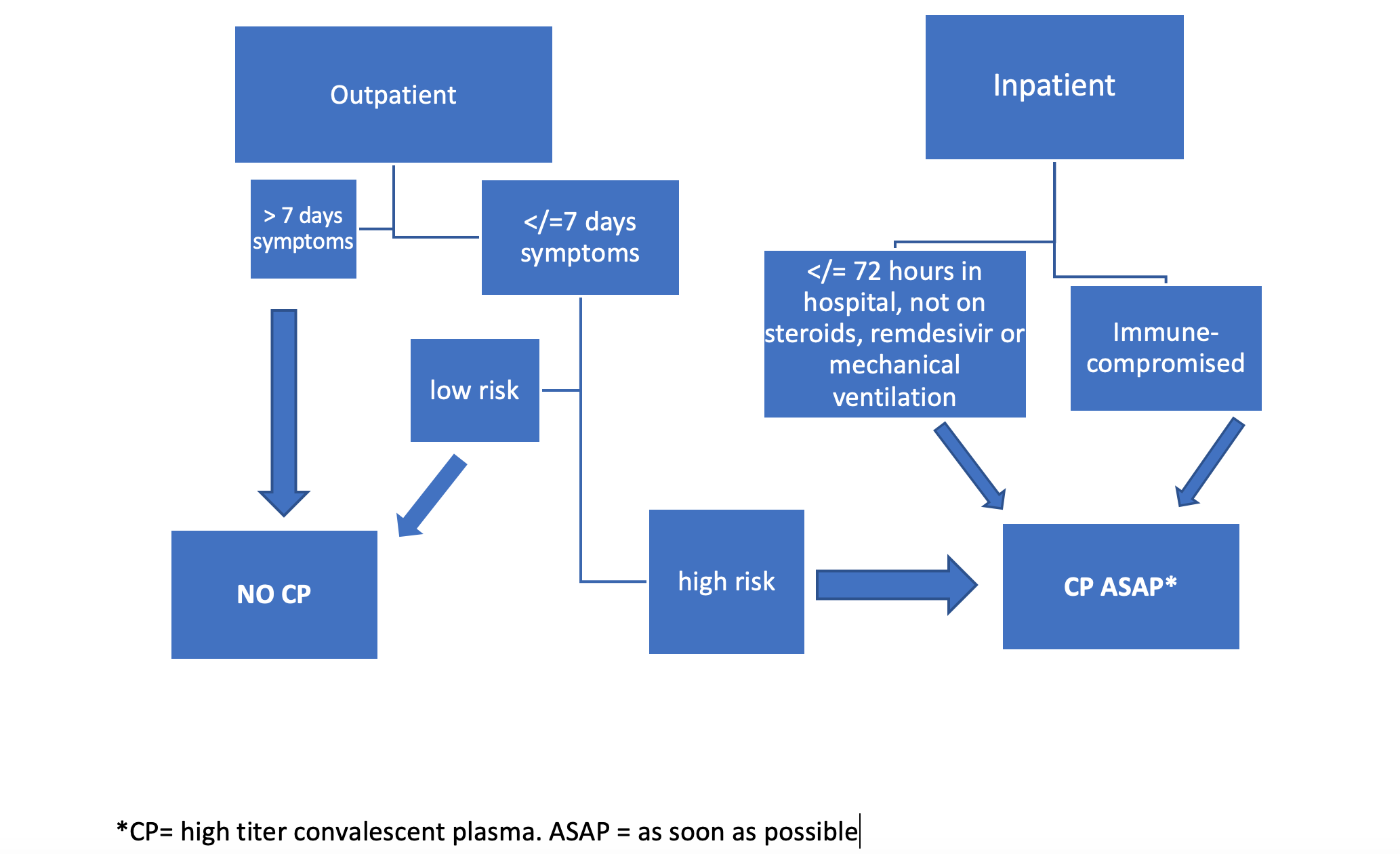 This flowchart shows different paths for convalescent plasma use in outpatient and inpatients individuals.
This flowchart shows different paths for convalescent plasma use in outpatient and inpatients individuals.